|
NW London System Update: November 2024
|
|
|
|
A message from Rob Hurd
Dear colleagues,
Welcome to the last ICS update of 2024. Due to the festive break towards the end of December, there will be no update next month. The next one will be circulated at the end of January 2025.
I want to thank everyone for your support and partnership working during 2024. It has been a challenging year with significant system pressures, exacerbated by industrial action and financial challenges across the system. In the ICB, we have been through a significant reorganisation to ensure we have the right structures and staffing in place to meet our strategic duties and objectives. We have published an updated Joint Forward Plan and we have been pleased that the objectives and approach set out in the emerging Ten Year Plan for the NHS align closely to what we were already doing in North West London.
This month we were delighted by the overwhelming response to our patient survey on access to primary care. Over 95,000 patients responded, which clearly illustrates the importance of the issue to our residents. We have also launched ‘Compassionate Care For All’, our public consultation on community-based palliative care services – please do help us to get the word out to local people and encourage as many residents as possible to take part. We also were proud to hold the second annual Health Equity Summit and Health Equity Awards: tackling health inequalities is a key objective of the ICS and our work in this area is a great example of the NHS and local authorities working together.
Wishing everyone a happy festive and New Year period – though I know I will speak to many of you in the weeks ahead!
Best wishes,
Rob
|
|
|
|
More than 95,000 patients in north west London responded to the recent survey on access to general practice. Results are now being analysed in detail and we will report them soon.
Furthermore, each of our 45 primary care networks (PCNs) are invited to hold at least two events to discuss access to services with their patients and local communities. We anticipate these will be held over the next few months. Funding is available for PCNs and practices that develop robust proposals to improve patient access. Any changes be co-designed and localised so they can best meet the needs of local residents.
|
The North West London Health Equity Summit took place on 18 November 2024, bringing together over 200 attendees to accelerate system learning and exchange best practices. This year's theme, Empowering Communities for More Equitable Health Outcomes, inspired insightful discussions and collaborative action toward reducing health disparities. The event celebrated excellence through the Health Equity Awards. Our six winners are:
- Ganesh Sathyamoorthy – Co-founder of the Ethnicity and Health Unit
- Resonate Arts – A local charity specialising in emotionally, culturally, and cognitively inclusive dementia-friendly sessions
- Sasha Nelson – Recognised for collaborative work using a co-production approach through community roadshows and smaller multi-faith health events
- Patricia Wharton – Known as Blaze, a radio presenter from The Let’s Talk Show and an ambassador for community cancer care
- Luxmi Dhoonmoon – Tissue viability nurse consultant, leading the implementation of a skin tone risk assessment tool to assess pressure ulcer risk for all skin tones
- The Wealdstone Baby Bank – For supporting parents in overcoming the negative effects of poverty.
|
2025/26 system planPlanning guidance for 2025/26 is expected by the end of December and the ICB has started work on developing our sector plan. While additional funding was allocated to the NHS in the Budget, the costs of system pressures and pay awards mean a real terms reduction in available funding. The ICB is under financial pressure in 2024/25 and recovery actions are underway to bring the spend in line with plan. A number of actions are non-recurrent and therefore an underlying deficit is forecast going into 2025/26. The ICB will not be issuing ‘commissioning intentions’ as we used to do when we were a CCG – our plans are set out in the Joint Forward Plan, which is agreed through the ICB Board and local Health and Wellbeing Boards. NHS Ten Year planColleagues may have read coverage in the media around the NHS Ten Year Plan, the process to agree this over the months ahead and the role of NHS England, Providers and ICBs in delivering. Amanda Pritchard, Chief Executive of NHS England, has written to ICB CEOs to clarify the position. The approach very much vindicates and supports our organisation redesign and operating model. The letter is clear that another large reorganisation is not happening. It states that ICBs are central to ‘self-managing, self-improving systems’ and critical to delivering the ‘three shifts’ the government is seeking: from treatment to prevention, from analogue to digital and from hospital to community. ICBs “will continue to be the system leader for the NHS, convening and working across all key partners within their integrated care system”. ICBs will continue to manage the performance of provider Trusts against the contracts we commission. NHSE’s role in this will be to step in where performance is below an acceptable level, and the use of commissioning levers (including the agreement of ICS strategy and ICS plans and programmes of work) has not secured improvement. The letter also confirms that ICBs will have “primary responsibility for ensuring the delivery of neighbourhood health, identifying population health needs and acting on reversible risk factors to improve healthy life expectancy and reduce utilisation of secondary care”. Again, this is entirely in line with our operating model and the fundamental role to empower borough-based Partnerships to enable and organise health and care services geared towards our neighbourhoods within the boroughs. An updated NHS Oversight and Assessment Framework will be issued shortly, underpinned this with a new NHS Performance, Improvement and Regulation Framework.
|
“Compassionate care for all” public consultation
|
NHS North West London is inviting local residents to share their views on proposed improvements to adult community specialist palliative care. The aim is to ensure compassionate, high-quality support for those facing serious or life-limiting illnesses. This pubic consultation takes place 18 November 2024 – 24 February 2025. Our proposal includes:
- 12-hour, 7-day specialist palliative care nursing teams in all boroughs
- 24/7 telephone advice line for immediate support
- Expanded "Hospice at Home" services
- Specialist outpatient clinics in each borough
- Improved access to psychological and bereavement support
- Enhanced lymphoedema care services (Lymphoedema is a long-term condition where a build-up of lymph fluid in your body's soft tissues causes swelling
- 46 new enhanced end-of-life care beds across the north west London Maintaining the existing 57 hospice inpatient beds.
Consultation options:
- Option A (Preferred): Implement the new model and add 46 enhanced end-of-life care beds without reopening Pembridge Palliative Care Centre Inpatient Unit beds.
- Option B: Implement the new model, add 46 enhanced end-of-life care beds, and reopen Pembridge Palliative Care Centre Inpatient Unit beds. This requires reducing hospice beds elsewhere.
We are inviting local residents to share their views at scheduled events that are taking place across our eight boroughs. Find out more here. |
Cancer services – potential relocation from Mount Vernon
|
NHS England is making plans to consult on proposed changes to Mount Vernon Cancer Centre (MVCC) services, including its relocation to an acute hospital site, Watford General Hospital. The aim is to enhance service safety, efficiency, and accessibility for the population currently served by Mount Vernon Cancer Centre including north west London patients. This work is led by NHS England, not NHS North West London, though we will support NHSE’s approach to consultation. Key Proposals1. Relocation to Watford General Hospital:
- Ensures access to co-located clinical services (e.g., critical care, A&E).
- To also be managed by a specialist provider (UCLH) to improve care quality and research access.
- Minimal travel time increase for north west London patients, with transport solutions under review.
2. Enhanced Local Access:
- Expansion of chemotherapy services at Northwick Park Hospital by adding three chairs initially, with future capacity to increase by 50%.
- Introduction of a chemotherapy-at-home service to improve convenience and reduce travel.
- Local blood testing facilities with results integrated across hospital systems.
3. Future Developments:
- Increased radiotherapy capacity at nearby locations.
- New networked radiotherapy unit (Luton/Stevenage) anticipated by 2027/28.
- New Chemotherapy Unit at Hillingdon Hospital as part of new hospital construction.
Rationale for ChangeAn independent clinical review in 2019 highlighted risks in maintaining current services, including lack of co-located critical services and workforce challenges. Relocation to Watford, supported by patient and public engagement, addresses these concerns while ensuring long-term sustainability. Health scrutinyA Joint Health Scrutiny Committee is being established between ten local authorities, including the London Boroughs of Harrow, Hillingdon, Brent and Ealing. It will be chaired by the Hertfordshire Health Scrutiny Chair with Hillingdon Health Scrutiny Chair in the role of vice chair. Its first meeting is scheduled to take place in mid-December 2024. Public ConsultationPlanned for early 2025 (subject to approval), the consultation will include:
- Face-to-face and online meetings
- Roadshows and themed workshops
- Engagement with community groups, faith organizations, and healthcare bodies
- Surveys and accessible information dissemination.
Next StepsNHS North West London working with NHS England to collaborate with stakeholders to support effective consultation, address concerns, and plan for service improvements ahead of the relocation. For more information, visit: www.mvccreview.nhs.uk. Background informationThe table below shows patient figures from all areas for the 2023/24 financial year (by former CCG area). 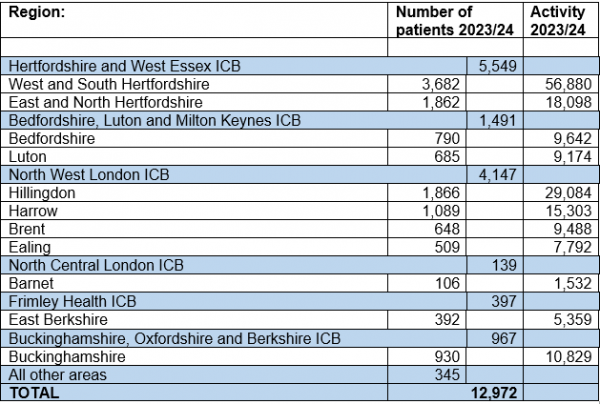 |
North west London had three winners in the Health Service Journal (HSJ) Awards 2024. These are listed below:
- Modernising Diagnostics Award - North West London Integrated Care System (North West London AcuPebble Pathway for Straight-to-Test Obstructive Sleep Apnoea Diagnosis: Faster, Cheaper, Equitable, and Sustainable Diagnostic Modernisation)
- Provider Collaboration of the Year - West London Trust and Central and North West London Trust (North West London CAMHS Specialised Commissioning Provider Collaborative)
- NHS Race Equality Award - The Royal Marsden (Breaking Barriers in Healthcare Inequality Through a UK-First Skin-Tone Inclusive Softie).
The North West London Refugee Employment Programme won NHS England's award for Collaboration and Partnerships for its work in supporting refugees access Healthcare Support Worker opportunities in the NHS. This was awarded to Nathan Christie-Plummer, Director of Workforce at West London NHS Trust, and Anthony Sembatya, Programme Manager, Refugee Employment Programme at NHS North West London. The Chiswick Primacy Care Network (PCN) Pharmacy Team was shortlisted for Pharmacist/Pharmacy Team of the Year Award. The Chiswick Primary Care Network Pharmacy Team has established itself as a valuable part of the local healthcare landscape, demonstrating the value of pharmacy teams in primary care. The team has driven innovation and made significant contributions to both patient care and staff development. Their team’s work has produced measurable improvements in patient outcomes. An example is the creation of the ‘blood pressure club’, an initiative designed to tackle undiagnosed and uncontrolled hypertension. By auditing established practices, gaps in how blood pressure was monitored and managed were identified. Through personalised invitations, the loaning of blood pressure machines and providing follow-up care, the team successfully improved hypertension detection and management across the patient population. The initiative has now been rolled out to all practices within the PCN, with the work reducing GP workloads and empowering patients through education and proactive follow-ups. |
Programmes and initiatives
|
WorkWell is a project bridging Employment and Health Equity in north west London by integrating health and employment support. This integration streamlines patient care and saves time for GP practices and Social Prescribers. We are sharing testimonials of how the health of people is improving though the personalised approach to removing health barriers to thriving at work. The initiative has shown strong initial traction, receiving 279 referrals in October 2024, primarily from Job Centre Plus partners. In our first month of operation, we exceeded our monthly target, achieving 114% of starts with 182 people beginning their WorkWell journey. The focus is now on increasing referrals from primary care by positioning WorkWell as a prescription for health outcomes. We have engaged with several boroughs to initiate promising pilots to drive referral growth, including:
- Development of patient-focused podcasts and webinars - Hounslow
- Partnerships with local MSK services - Hounslow
- Analysis of Med3 data through EMIS - Harrow
- Video - How to refer into WorkWell from a GPs perspective – Westminster.
There are promotional events to demonstrate the ease of referrals into WorkWell, and a podcast with a participant and Work and Health Coach. We are commencing a four-month pilot work to reach specific groups in our communities, including health-focused communities and faith-based outreach. |
The Hounslow Integrated Discharge Hub which is responsible for the seamless transfer of patients’ care and support into the community, scored outstandingly high on the recent Transfer of Care Hub (ToCH) maturity matrix based on the following.
- The high level of partner integration in the hub
- 7-day functionality
- Strong leadership with clinical input into the transfer function
- Detailed development on progressing maturity since the self-assessment in 2023.
This development is underpinned by robust data collection (analysis and insight); the innovative ‘Pentagon Model’ (a uniquely designed model for the multi-disciplinary triage of Pathway 1 referrals that’s takes place twice a day, seven days a week) and a strong link with the Hounslow Borough Based Partnership leadership team who help the hub to address barriers and identify opportunities. Since the ‘Pentagon Model’ came into effect because of the new Bridging Care scheme in November 2023, there has been an improvement in delay days by 0.5 days for faster discharges of Pathway 1 patients. |
|
Work on the revised NHS North West London Estates Infrastructure Plan and North West London ICS Estates Strategy is drawing to a conclusion with plans to progress this through internal governance this quarter. This follows ongoing engagement with Trusts, local authority and borough representatives. The emerging strategy seeks to make more effective use of our existing estate and that belonging to our local authority/public sector partners. The strategy will be informed by broader clinical, acute and primary care strategies. It will seek to prioritise a number of sites and projects that will enable ICS priorities whilst ensuring our estate remains sustainable, resilient, able to accommodate Integrated Neighbourhood Teams and other clinical activity, and provides improved access to care.
Estates rationalisation has now concluded across the eight boroughs. We thank all borough-based teams for their continued collaboration at this time. The focus will now move to improving utilisation of space at Marylebone Road and supporting teams with returning to the office.
Work progresses with ICS partners to inform local authority Local Plans and their respective Infrastructure Delivery Plans (IDPs). Hounslow and Harrow IDP submissions have now been completed, with preparations being made within NHS North West London to submit bids for external funding (Community Infrastructure Levy, CIL), which is linked to this process. Further discussions are currently underway with Brent and Kensington & Chelsea local authorities around bidding for additional CIL funding to enable projects identified under the strategy and mitigate the impact of population growth across boroughs. It has been confirmed that north west London have been able to obtain the biggest CIL and s106 (external funding) allocation across all London ICBs. The allocation of this funding will be allocated accordingly in alignment with Estates Strategy needs.
NHS North West London Estates team continue to meet regularly with NHS property companies (NHS Property Services and CHP) to undertake audits and review occupancy, lease management and charging across all sites. Feasibility and utilisation studies are commencing at St Charles, Heart of Hounslow, Willesden Centre for Health and The Meadows, some of our costliest and underutilised estate, to explore new opportunities for optimisation and reducing significant ‘void’ costs to NHS North West London.
Estates projects due to complete this financial year include the Hillcrest Surgery relocation and refurbishment (Dec 24/Jan 2025 - Ealing), expansion of primary care and reduction in underutilised space at Grand Union Village (Dec 24 - Ealing), and the delivery of a new primary care facility in South Kilburn (Mar/Apr 25 - Brent).
Estates are working closely with the trusts’ sustainability leads and the national Greener NHS Programme Team to prioritise and progress sustainability activity across north west London. The first Sustainability Update was shared with the ICS Leadership this month to raise awareness of the excellent working being undertaken by Trusts and other ICS partners to reach our Net-Zero Carbon ambitions.
Applications for London Improvement Grant funding for FY 24/25 are now moving through final due diligence stages (to conclude 22nd Nov). Once final approval has been granted, second priority schemes will receive the go ahead to progress to delivery.
|
|
|
|
|